Last Updated:
January 15th, 2025
Have you ever heard of the phrase “Seeing pink elephants”? You may have noticed this unusual reference in conversations or mentioned it in the media. But have you ever wondered about the story behind this strange choice of animal and colouring? Why does it seem so closely tied to the concept of being drunk?
Initially, the origins of ‘seeing pink elephants’ may seem innocent, but once we scratch away at the surface, it uncovers a pretty disturbing history. In today’s blog, we dive into delirium tremens, its connection to seeing pink elephants, and, more importantly, how it relates to alcohol addiction.
Why ‘Pink Elephant’ specifically?
The idea of pink elephants symbolising hallucinations from alcohol originates in popular culture, and the imagery is linked to severe alcohol withdrawal symptoms known as delirium tremens (DT). The phrase’s exact origin is unclear, but it became well-known through various cultural references and artistic interpretations.
One idea is that ‘seeing pink elephants’ was a way to describe the incredibly frightening hallucinations people going through DT had. Imagine experiencing this in the early 1900s when knowledge, and more importantly, the treatment of alcoholism, was in its infancy. Pink elephants sound quite reassuring.
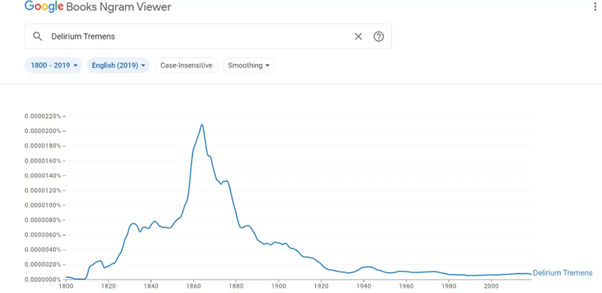
As we can observe from Google Books Ngram Viewer, the phrase’s recorded usage in books began in the early 1930s and experienced a significant surge in popularity around 1940.
So, what caused this sudden increase in the use of the phrase ‘pink elephants’?
Pink elephants and delirium tremens in popular culture
A turning point in the cultural adoption of ‘pink elephants’ was the release of the Disney movie “Dumbo” in 1941. In this animated classic, the young elephant Dumbo accidentally consumes alcohol and experiences a vivid hallucination featuring pink elephants. The film’s popularity solidified the connection between pink elephants and alcohol-induced hallucinations in the public consciousness.
In fact, the concept of pink elephants has been a recurring theme in popular culture over the years.
Above, we can see Barney, an alcoholic character from ‘The Simpsons,’ experiencing alcohol hallucinations with references to a pink elephant.
There’s even a brand of beer called ‘Delirium Tremens’, with the logo being a… You guessed it, a pink elephant.
We see it again in Disney’s House of Mouse cartoon series. Notice how the pink elephant ‘waiter’ seems to be drinking some form of alcohol!
But it doesn’t just stop at film and TV; pink elephants and delirium tremens are heavily used in songs throughout history:
Northern Irish band The Divine Comedy had this to say on the appropriately named ‘A Drinking Song’;
We’ll drink beyond the boundaries of sense!
We’ll drink ’til we start to see lovely pink elephants;
Inside our heads, inside our beds,
Inside the threads of our pyjama legs!
So don’t shoot ’til you see the reds of our eyes,
And an army of elephants marching behind!
But should all of this be taken as lightly as it’s portrayed in the media? Is it all a ‘bit of a laugh’ to experience hallucinations from alcohol abuse? The answer to both these questions is a resounding; ‘No’.
A closer look at delirium tremens and alcohol withdrawal
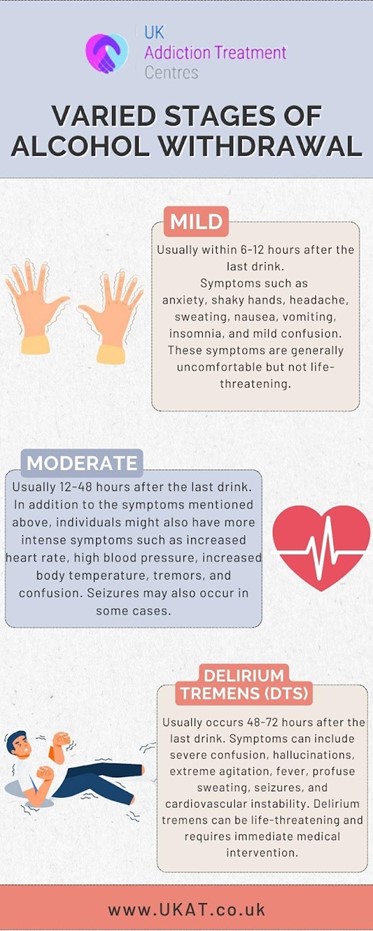
Despite how it’s portrayed in the media, DT is a severe and potentially life-threatening syndrome. Alcohol withdrawal refers to the physical and psychological symptoms that can occur when an individual dependent on alcohol suddenly stops or reduces their alcohol consumption.
These symptoms can range from mild to severe and even life-threatening in some cases. Medical professionals often categorise alcohol withdrawal into different severities based on the intensity of the symptoms.
Delirium tremens is characterised by a combination of physical and psychological symptoms, which typically develop within 48 to 72 hours after the last alcoholic drink. Let’s take a closer look at these symptoms:
- Delirium: Profound confusion, disorientation, and altered mental state are hallmark features of delirium tremens. Individuals may have difficulty recognising people or their surroundings.
- Tremors: Severe trembling of the hands and sometimes the whole body is a prominent symptom, where the name “delirium tremens” originates.
- Hallucinations: Visual and auditory hallucinations are common during DTs. People may see or hear things not there, contributing to their confusion and distress.
- Agitation: Restlessness, irritability, and agitation are often present in individuals experiencing DTs.
- Autonomic hyperactivity: Individuals with DTs may experience symptoms such as rapid heart rate (tachycardia), high blood pressure (hypertension), sweating, and fever.
- Seizures: Seizures can occur in severe cases of DTs, which can further complicate the condition.
- Altered consciousness: People with delirium tremens may have altered levels of consciousness, ranging from stupor to agitation.
- Severe anxiety: Intense anxiety and fear are common during DTs.
If you notice yourself or others experiencing any of these symptoms, dial 999 and get help immediately.
The science behind delirium tremens- why does it happen?
It may surprise you that something so freely available in supermarkets across the globe can harm the body so severely. Even the slightest glance at the list of symptoms shows how serious DT can be, but what causes this reaction? Well, we need to get a little ‘science-y’.
Alcohol initially calms the brain by boosting a relaxing neurotransmitter called GABA while lowering the activity of an excitatory transmitter called glutamate. However, with prolonged alcohol use, the brain adapts by becoming more sensitive to keep an even balance.
When alcohol is suddenly stopped, GABA’s calming effects decrease, increasing brain activity. This spike in neural activity causes the troubling symptoms of DT, like hallucinations and instability.
Recognising these brain chemistry changes helps explain why DT occurs during alcohol withdrawal, emphasising the vital role of medical care and support during this difficult time.
Who is most at risk for experiencing delirium tremens?
While it’s worth noting that not everyone withdrawing from alcohol experiences DT, some people are at a higher risk of experiencing it than others:
- Heavy and prolonged alcohol use: Individuals who have been consuming alcohol heavily and for an extended period are at the highest risk. Chronic alcohol abuse can lead to physical dependence on alcohol, making withdrawal symptoms, including DT, more likely when alcohol consumption is suddenly reduced or stopped.
- Previous episodes of DT: If someone has experienced DT during a previous episode of alcohol withdrawal, they are at a higher risk of developing it again during subsequent attempts at quitting alcohol.
- Coexisting medical conditions: Individuals with other medical conditions, such as liver disease, pancreatitis, cardiovascular disease, or a history of seizures, may be more susceptible to DT during alcohol withdrawal.
Longevity and mortality rate- Quick Fire Facts
- DT is usually short-lived, typically spanning 3 to 4 days but sometimes extending to as long as eight days. It typically ends with an extended period of sleep.
- The chance of experiencing DT in individuals with alcohol abuse issues typically falls between 5% and 10%, according to research.
- DT can extend hospitalisation periods, ICU stays, and the likelihood of mortality. Notably, mortality rates associated with DT have considerably diminished over time, particularly with the introduction of benzodiazepines as a treatment for alcohol withdrawal.
- The mortality rate falls from 1% to 4%, and timely intervention can further reduce this risk.
How can I get help for alcohol addiction?
At UKAT clinic, we understand the challenges people face when dealing with alcohol addiction. Our inpatient detox clinics provide a safe and compassionate haven for your recovery journey.
With round-the-clock medical supervision and specialised care, including medications to manage severe withdrawal symptoms like delirium tremens, you’ll find comfort in knowing that your health is our top priority.
Our controlled environment minimises the risk of DT-related complications, offering you peace of mind. Beyond that, our dedicated team offers structured support and therapy to help you address the underlying causes of your addiction, setting you on a path towards lasting recovery.
Your well-being matters to us, and we’re here to support you every step of the way.